Vasectomy is one of the most widely performed surgical procedures for permanent male contraception. With its minimally invasive nature and high effectiveness, vasectomy has become a cornerstone of family planning. However, alongside its popularity, questions often arise about the long-term implications of vasectomy, particularly concerning testicular function. Men often wonder: Will vasectomy affect my testosterone levels? Does sperm production continue after the procedure? Could there be testicular atrophy or dysfunction years later?
This article explores these questions in depth, examining how vasectomy interacts with testicular physiology, what clinical research reveals about long-term outcomes, and what men should consider when weighing their options.
Understanding Testicular Function Before Vasectomy
To appreciate the long-term effects, it is essential to first understand the role of the testes. The testes serve two primary functions:
- Spermatogenesis – The production of sperm within the seminiferous tubules.
- Hormone production – Primarily testosterone, secreted by Leydig cells.
Testosterone influences male sexual development, libido, muscle mass, bone health, and mood regulation. Spermatogenesis, meanwhile, ensures fertility by generating mature sperm capable of fertilizing an egg.
Vasectomy/ does not remove the testes or affect their blood supply, so the fundamental structure of testicular function remains intact after surgery. But the key question is whether changes occur over time.
What Happens in the Testes After Vasectomy?
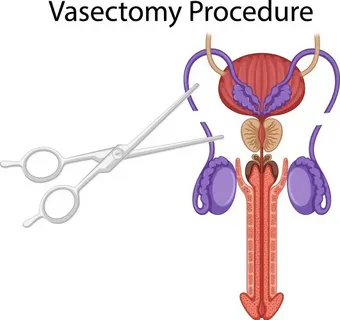
During a vasectomy, the vas deferens—the tubes that transport sperm from the epididymis to the urethra—are cut, sealed, or blocked. This prevents sperm from mixing with semen during ejaculation.
Post-vasectomy, the following changes typically occur in the testes:
- Sperm production continues: The testes do not stop producing sperm; instead, sperm are reabsorbed by the body when they can’t pass through the vas deferens.
- Pressure changes in the epididymis: Blockage may cause mild dilation of the epididymal tubules.
- Formation of sperm granulomas: Small inflammatory nodules may form as the body reacts to leaked sperm.
- Immune response: Some men develop anti-sperm antibodies as the immune system encounters sperm proteins.
These responses are natural adaptations. The important consideration is whether they compromise testicular function in the long run.
Vasectomy and Hormonal Function Over Time
One of the most common concerns among men is whether vasectomy affects testosterone production. Multiple studies have investigated this question, and the consensus is clear:
- Testosterone production is not impaired by vasectomy. The Leydig cells continue functioning normally.
- Longitudinal studies show no decline in circulating testosterone levels after vasectomy compared with age-matched controls.
- Other hormones, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH), also remain stable.
In fact, some research suggests that sexual function and libido may even improve in certain men after vasectomy, largely because anxiety about unintended pregnancy is reduced.
Vasectomy and Spermatogenesis Over Time
Although the testes continue to produce sperm after vasectomy, there are unique long-term considerations:
- Sperm production persists at normal rates, but mature sperm cannot exit the testes.
- Over time, the epididymal tubules may distend slightly due to sperm accumulation.
- In some men, spermatogenesis slows modestly with age, but this is part of normal aging, not vasectomy.
- Studies using testicular biopsies have shown no significant histological damage decades after vasectomy.
Thus, while the pathway for sperm release is blocked, the fundamental process of sperm creation remains unaffected.
Testicular Structure and Blood Flow After Vasectomy
Another area of investigation is whether vasectomy impacts the physical structure or blood supply of the testes.
- Blood flow studies using Doppler ultrasound have found no clinically significant reduction in testicular perfusion after vasectomy.
- Size and volume of testes remain stable in long-term follow-up, with no consistent evidence of atrophy.
- Occasional cases of scarring or fibrosis at the epididymis may occur, but this does not usually impair testicular function.
Overall, the testes adapt well without structural compromise.
Vasectomy and Testicular Pain Syndromes
Although vasectomy does not directly impair testicular function, some men report chronic testicular pain, known as post-vasectomy pain syndrome (PVPS).
- PVPS occurs in approximately 1–2% of men.
- Causes include nerve irritation, epididymal congestion, or sperm granulomas.
- In severe cases, surgical intervention such as vasectomy reversal or epididymectomy may be required.
It is important to note that while PVPS can impact quality of life, it does not equate to testicular dysfunction.
Vasectomy and Autoimmune Reactions
When sperm are trapped inside the testes and epididymis, some sperm proteins may leak into surrounding tissues. Because sperm are normally protected by the blood-testis barrier, the immune system may recognize them as foreign.
- Anti-sperm antibodies are found in 50–70% of men after vasectomy.
- These antibodies do not appear to impair testicular hormonal function.
- However, they may complicate fertility if reversal is attempted, since they can affect sperm motility.
This demonstrates that while the testes continue functioning, immune adaptations can influence fertility outcomes.
Vasectomy and Aging of Testicular Function
As men age, testicular function naturally changes. It is important to separate age-related changes from those caused by vasectomy.
- Testosterone levels gradually decline with age (around 1% per year after 30). Vasectomy does not accelerate this decline.
- Sperm production decreases with age, even in men without vasectomy.
- Vasectomy and aging combined do not show synergistic effects; the decline is attributed primarily to aging itself.
Thus, vasectomy does not speed up the normal aging process of the testes.
Clinical Evidence: Long-Term Studies
Several landmark studies have investigated the long-term outcomes of vasectomy on testicular function:
- The Oxford Family Planning Association Study – Followed thousands of men for over two decades and found no evidence of impaired testicular function.
- World Health Organization multicenter trials – Reported that vasectomy had no significant impact on testosterone, LH, or FSH.
- Biopsy-based research – Demonstrated preserved testicular histology up to 20 years post-vasectomy.
These studies reinforce the conclusion that vasectomy does not damage the testes over time.
Psychological Impact and Perceptions of Testicular Health
While physiology remains stable, men’s perceptions about their testicular health may change after vasectomy.
- Some men report heightened awareness of testicular sensations.
- Anxiety about long-term health risks can influence perception of pain or dysfunction.
- Counseling before vasectomy can help manage expectations and reassure men about long-term outcomes.
Key Takeaways
- Hormonal function remains intact after vasectomy, with no decline in testosterone linked to the procedure.
- Spermatogenesis continues, though sperm are reabsorbed rather than ejaculated.
- No evidence of testicular atrophy or impaired blood flow has been found in long-term studies.
- Autoimmune changes may occur but do not compromise testicular health, though they can influence fertility if reversal is sought.
- Chronic pain is rare, but when present, it affects quality of life more than testicular function itself.
Conclusion
Vasectomy is a safe, effective, and permanent method of contraception that does not impair testicular function over time. Both hormone production and sperm generation continue normally, with adaptations that the body manages effectively. Concerns about testicular atrophy, hormonal imbalance, or loss of masculinity are not supported by scientific evidence.
For men considering vasectomy, understanding these facts is crucial. Long-term research confirms that testicular health remains preserved, making vasectomy a reliable choice for those seeking permanent contraception.
FAQs
1. Does vasectomy lower testosterone levels over time?
No. Vasectomy does not affect Leydig cell function, which produces testosterone. Multiple long-term studies have confirmed that testosterone levels remain stable after vasectomy, with changes attributed to normal aging rather than the surgery.
2. Can vasectomy cause testicular atrophy or shrinkage?
There is no evidence that vasectomy causes testicular atrophy. Testicular size and volume remain consistent over time, with no reduction in blood supply or tissue integrity.
3. Does vasectomy stop sperm production in the testes?
No. Spermatogenesis continues at normal rates after vasectomy. The difference is that sperm cannot travel through the vas deferens, so they are instead reabsorbed by the body. This natural process does not harm testicular function.